HPV is common. Confusion about it is common too. Let’s separate facts from noise so you can make decisions that protect your health. You’ll learn what HPV is, what the vaccine does (and doesn’t do), who should get it, and what to ask your healthcare provider.
Quick Facts
HPV is extremely common, and most sexually active people will be exposed at some point.
The HPV vaccine is safe and effective at preventing HPV-related cancers.
The vaccine works best before exposure to HPV, but some people can still benefit later.
HPV Basics
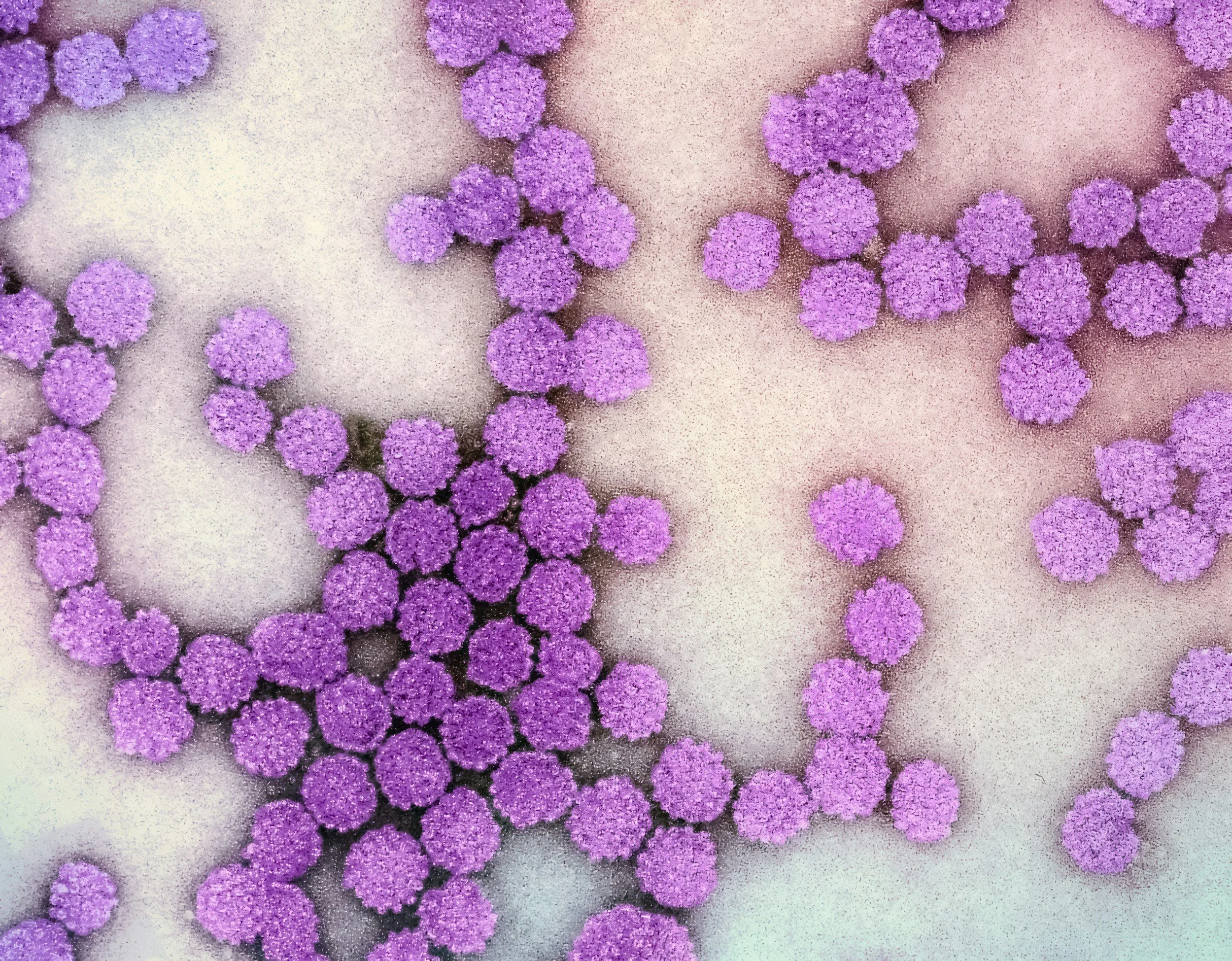
HPV (human papillomavirus) is a group of viruses. Some types are “low-risk” (they can cause genital warts). Other types are “high-risk” (they can lead to cancers, including cervical, anal, penile, vulvar, vaginal, and some throat cancers).
Most people who get HPV never know it. Your body often clears it on its own. But when high-risk HPV sticks around for years, it can cause cell changes that may turn into cancer.
Myths vs Facts
-
Fact: HPV is common. Exposure can happen with any sexual history, including with a small number of partners.
HPV is not a character flaw. It’s a virus.
-
Fact: HPV affects everyone. Vaccination is recommended for all genders and helps prevent multiple cancers.
-
Fact: The vaccine works best before exposure to HPV, which is why it’s recommended at younger ages.
-
Fact: There is no credible evidence that the HPV vaccine causes infertility. Safety monitoring continues to show the HPV vaccine is safe.
-
Fact: HPV vaccines have been studied extensively and are continuously monitored for safety.
-
Fact: The vaccine does not treat existing HPV, but it can still protect against HPV types you have not been exposed to. Talk with a clinician about what makes sense for you.
-
Fact: Vaccination is powerful prevention, but routine screening (like cervical cancer screening when appropriate) still matters.
-
Fact: The vaccine prevents cancer by protecting against a common virus. Medical organizations recommend it because it works best before exposure.
-
Fact:The most common side effects are typically mild (like a sore arm). Serious allergic reactions are rare, and vaccine safety is continuously monitored.
Who should get the HPV vaccine?
Ages 11-12 (can start as early as 9)
Through age 26: Catch-up vaccination if not adequately vaccinated.
Ages 27-45: not routine for everyone, but may be considered. Talk with your healthcare provider.
What to Ask Your Healthcare Provider
“Am I vaccinated against HPV? If not, should I start the series now?”
“If I’m 27–45, would I personally benefit from vaccination?”
“What cancer screenings do I need based on my body and my risk factors?”
“If I’ve had abnormal results before, what follow-up plan should I be on?”
